Vasectomy and Nerve-Sparing Treatment Techniques
Vasectomy is one of the most effective and widely performed methods of permanent male contraception. With advancements in surgical technique, anesthesia, and post-operative care, modern vasectomy has evolved into a minimally invasive, highly precise procedure with excellent safety outcomes. Among the most important developments in recent years is the growing emphasis on nerve-sparing treatment techniques. These approaches aim to reduce post-procedural pain, minimize complications, and improve overall patient satisfaction without compromising the effectiveness of the vasectomy.
Understanding how nerve-sparing principles are applied during vasectomy helps patients and clinicians alike appreciate why contemporary outcomes are significantly better than those seen decades ago.
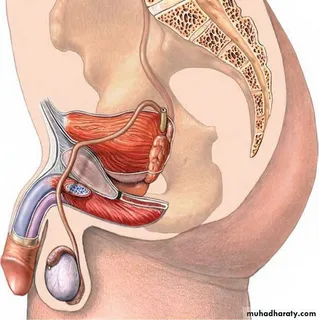
Understanding Nerve Anatomy in Vasectomy
To appreciate nerve-sparing vasectomy techniques, it is essential to understand the basic nerve anatomy of the scrotum and spermatic cord. The scrotal contents are innervated by branches of several nerves, including:
- The ilioinguinal nerve
- The genital branch of the genitofemoral nerve
- Posterior scrotal nerves from the pudendal nerve
- Fine autonomic nerve fibers traveling alongside the vas deferens
These nerves are responsible for sensation, temperature regulation, and reflexive muscular responses. During vasectomy, the vas deferens is isolated and interrupted. Traditional techniques sometimes involved extensive tissue handling, traction, or cauterization near these neural pathways, which could increase the risk of nerve irritation or injury.
Nerve-sparing treatment techniques focus on precise dissection, limited tissue trauma, and targeted anesthesia, all designed to preserve surrounding neural structures.
Evolution of Nerve-Sparing Vasectomy Approaches
Earlier vasectomy methods were effective but occasionally associated with higher rates of post-operative discomfort and, in rare cases, chronic pain. As urologic research progressed, surgeons began refining their approach to minimize unnecessary disruption.
Key milestones in the evolution of nerve-sparing vasectomy include:
- The adoption of no-scalpel vasectomy techniques
- Improved understanding of perivasal nerve distribution
- Use of fine instruments and magnification
- Development of targeted anesthetic delivery methods
These innovations collectively shifted vasectomy from a purely mechanical interruption of the vas deferens to a tissue-respecting microsurgical procedure.
Core Principles of Nerve-Sparing Treatment Techniques
Nerve-sparing vasectomy is not a single technique but a collection of guiding principles applied throughout the procedure.
Minimal Tissue Dissection
One of the most important principles is limiting dissection to only what is necessary. Excessive separation of tissues increases the likelihood of nerve irritation and post-operative inflammation.
By isolating the vas deferens through a small puncture or minimal incision, surgeons avoid disturbing adjacent nerve fibers embedded in the spermatic cord.
Gentle Vas Handling
Traction on the vas deferens can transmit force to surrounding nerves. Nerve-sparing treatment techniques emphasize gentle handling, using fine instruments to stabilize rather than pull aggressively.
This approach reduces mechanical stress on neural structures and lowers the risk of neuritis.
Precise Hemostasis
Bleeding control is critical in any surgical procedure. However, excessive cauterization near nerve-rich areas can lead to thermal injury.
Nerve-sparing vasectomy relies on:
- Low-energy cautery when necessary
- Mechanical ligation or clips
- Focused application away from neural pathways
Role of Targeted Anesthesia in Nerve Preservation
Anesthesia plays a major role in nerve-sparing vasectomy. Modern approaches go beyond simple local infiltration.
Perivasal Anesthetic Blocks
Instead of flooding the entire scrotal area with anesthetic, clinicians may use perivasal blocks. These involve injecting anesthetic precisely around the vas deferens, reducing pressure and chemical irritation to nearby nerves.
Buffering and Warming Anesthetics
Buffered and warmed anesthetic solutions reduce injection pain and local tissue irritation. This seemingly small adjustment contributes significantly to patient comfort and nerve preservation.
Avoidance of Excess Volume
Large volumes of anesthetic can increase tissue pressure, temporarily compressing nerve fibers. Nerve-sparing techniques emphasize using the lowest effective volume.
Nerve-Sparing Techniques in No-Scalpel Vasectomy
The no-scalpel vasectomy (NSV) approach naturally aligns with nerve-sparing principles. Instead of making incisions, the surgeon uses a sharp dissecting forceps to gently spread tissue layers.
Benefits of NSV related to nerve preservation include:
- Reduced disruption of superficial nerve endings
- Lower rates of hematoma and inflammation
- Faster sensory recovery
- Less post-operative pain
Because NSV limits tissue trauma, it is often considered the gold standard for nerve-sparing vasectomy.
Managing the Vas Without Neural Injury
Once isolated, the vas deferens must be occluded. Several occlusion methods exist, and nerve-sparing considerations influence the choice and execution.
Fascial Interposition
Fascial interposition places a tissue barrier between the cut ends of the vas deferens. When performed carefully, this method avoids excessive manipulation and reduces the need for aggressive cautery.
Thermal Cautery With Precision
When cautery is used, nerve-sparing treatment techniques prioritize:
- Short activation times
- Focused application inside the vas lumen
- Avoidance of surrounding tissue contact
Clip-Based Occlusion
In select cases, vas clips may be used to reduce thermal exposure. While clips are not suitable for all patients, they offer another nerve-conscious option.
Prevention of Post-Vasectomy Pain Syndrome (PVPS)
Post-vasectomy pain syndrome is a rare but impactful condition characterized by persistent scrotal discomfort lasting longer than three months. While its causes are multifactorial, nerve irritation is a recognized contributor.
Nerve-sparing treatment techniques reduce PVPS risk by:
- Minimizing neural trauma
- Reducing inflammatory responses
- Preventing neuroma formation
- Avoiding excessive scarring
Studies suggest that meticulous surgical technique and gentle tissue handling are among the most important factors in preventing chronic pain.
Post-Operative Care and Nerve Recovery
Nerve-sparing treatment does not end when the procedure is complete. Post-operative management plays a critical role in protecting healing nerve fibers.
Controlled Activity Restriction
Early overactivity can exacerbate inflammation around sensitive neural structures. Clear guidance on rest and gradual return to activity supports nerve recovery.
Anti-Inflammatory Strategies
Short courses of NSAIDs, ice application, and scrotal support help reduce swelling and nerve irritation during the initial healing phase.
Early Recognition of Neural Symptoms
Prompt evaluation of symptoms such as persistent burning, tingling, or radiating pain allows early intervention, often preventing progression to chronic pain.
Patient Selection and Counseling
Not all patients have the same nerve sensitivity or risk profile. Nerve-sparing vasectomy techniques are particularly valuable for:
- Patients with prior scrotal surgery
- Those with a history of chronic pain conditions
- Athletes or physically active individuals
- Patients expressing anxiety about pain outcomes
Pre-procedure counseling helps align expectations and reassures patients that modern vasectomy prioritizes comfort and long-term well-being.
Training and Surgeon Expertise
Successful nerve-sparing vasectomy depends heavily on surgeon skill. Familiarity with scrotal anatomy, experience with no-scalpel techniques, and attention to detail all influence outcomes.
Many urologists now receive specific training focused on:
- Microsurgical principles
- Pain-minimization strategies
- Advanced anesthesia techniques
This emphasis reflects a broader shift toward patient-centered surgical care.
The Future of Nerve-Sparing Vasectomy
Ongoing research continues to refine nerve-sparing treatment techniques. Emerging developments include:
- Ultrasound-assisted vas localization
- AI-guided procedural planning
- Enhanced nerve-mapping tools
- Personalized pain-risk assessment models
These innovations aim to further reduce complications while maintaining the effectiveness that makes vasectomy a trusted contraceptive option.
Conclusion
Vasectomy and nerve-sparing treatment techniques represent a significant advancement in male reproductive healthcare. By prioritizing precision, gentle tissue handling, targeted anesthesia, and thoughtful post-operative care, modern vasectomy minimizes nerve injury and enhances patient comfort.
For patients considering vasectomy, understanding the role of nerve-sparing techniques provides reassurance that the procedure is not only effective but also designed with long-term quality of life in mind. As surgical science continues to evolve, nerve preservation will remain a cornerstone of best-practice vasectomy care.
FAQs
1. What does nerve-sparing mean in vasectomy?
Nerve-sparing in vasectomy refers to surgical techniques that minimize disruption to the nerves surrounding the vas deferens. This approach reduces pain, lowers complication rates, and supports faster recovery.
2. Do nerve-sparing vasectomy techniques reduce chronic pain risk?
Yes. While chronic pain after vasectomy is uncommon, nerve-sparing techniques significantly reduce the risk by limiting nerve irritation, inflammation, and scarring.
3. Is nerve-sparing vasectomy as effective as traditional methods?
Absolutely. Nerve-sparing vasectomy maintains the same high effectiveness in preventing pregnancy while offering improved comfort and recovery outcomes